Dr Sylvain Chamberland, Orthodontiste says:
Thank you Dr Sajeva for your questions.1- Patients enrolled: All patients had a cl I occlusion and had their orthodontic treatment completed or within 2-3 months of completion. This is true for the 3 experimental groups.
2- There was no other skeletal deformity than vertical excess at the symphysis or lack of AP chin projection or both.
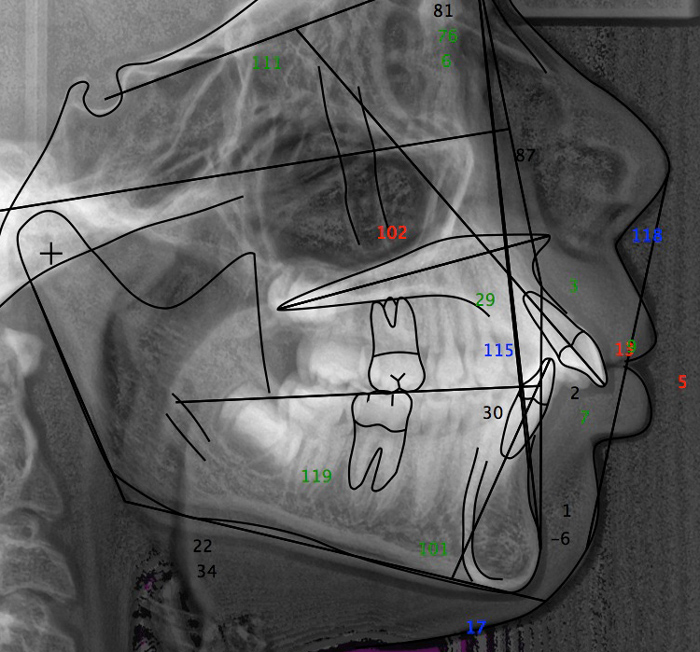
3-Hyperdivergent? The mean FMA was 34,06° (gr 1), 32,46° (gr 2), 34,76° (gr 3), 31,97° (Gr control). There was no statistical difference between groups regard FMA.
4- Unfavourable growth pattern.
This is answered in the discussion: "Does repositioning the chin have a deleterious effect on mandibular growth? That is a valid concern and has been a major reason for delaying it until growth is essentially completed...In a growing individual with an indication for forward-upward genioplasty, data from our control group show that lip incompetency persists, facial convexity is maintained, bone resorption occurs at point B, and symphysis thickness has a tendency to decrease.
Our data show that the growth pattern do not change after a genioplasty, ie a vertical growth pattern do not become an horizontal growth pattern.
5- Repropose genioplasty.
No patient had to undergo a second genioplasty. However, if a patient have juvenile rhumatoid arthritis and has condylar resorption, he might benefit from an early genioplasty and a revision when growth is completed if a 2nd surgical phase is indicated.
6- Case selection: case selection was rigorous.
"For all subjects, the recommendation for genioplasty was based on clinical evaluation of the prominence and vertical position of the soft tissue chin relative to the lips and midface. Cephalometric data for pretreatment a-p chin deficiency relative to the lower incisors, the vertical distance from the incisors to the bottom of the chin, and the mandibular plane angle are shown in Table 1."
Warm regards
Dr Sylvain Chamberland