Good morning Dre Roy,
I apologize for taking so long to answer. I was busy in the last few days.
I take note of your comment about "preconceived ideas". An exhaustive research published in the Cochrane library was precisely performed to find an answer to the preconceived idea that occlusal adjustments can treat or prevent symptoms or temporomandibular disorders.
But let's first differentiate two concepts:
1-Experience-based view.
Clinical experience and years of experience are the only important things for the practitioner. Usefulness of science is often denied. Anecdotal evidences are sufficient to make a clinical decision and are better than science. TMD diagnosis is based on meticulous analysis of occlusion. Recommendation is to use occlusion protected by the canine. Any position of the condyle other than supero-antero-medial position causes TMD. The use of articulators in orthodontics is favored.
2-Evidence-based view.
Science and scientific method are important to the practitioner. Benefit and usefulness of science are proven. Testimonies, case studies and non-objective experience are inadequate or insufficient to make a clinical decision. No definitive tests exist in TMD diagnosis. The gold standard for diagnosis is based on case story, clinical examination and TMJ imaging when indicated. Occlusion is not the main cause of TMD, but possibly plays a minor role in its etiology. TMD are a whole, a collection of disorders. The position of the condyle per se is not directly associated with TMD. Biological concept of a functional occlusion includes all kinds of occlusion (group function or canine guidance) but not occlusal interferences (balancing and protusion contacts are tolerated). Articulators are not necessary in orthodontics.
Rinchuse DJ, and Kandasamy S. Evidence-based versus experience based views on occlusion and TMD. AJODO 2005, feb;127(2):249-54
I would like to point out that even if I am a practitioner cumulating 30 years of experience, I am part of those who believe in evidence-based dentistry.
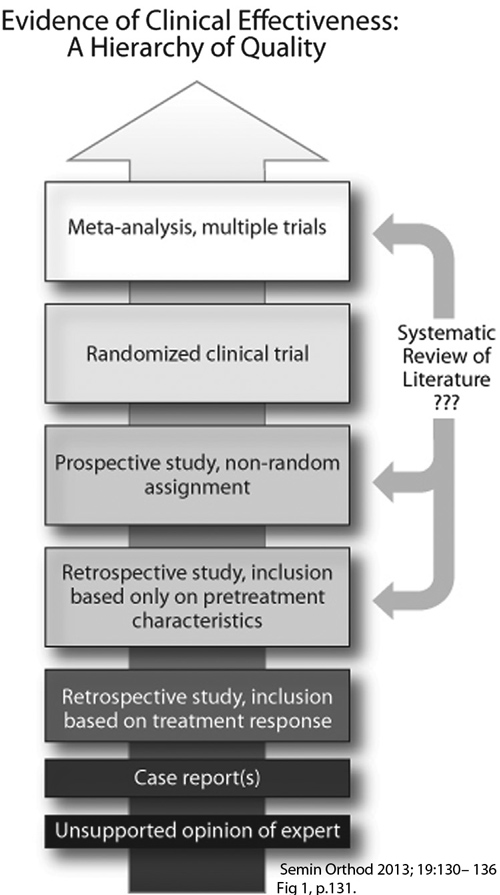
Hierarchy of quality of scientific evidence
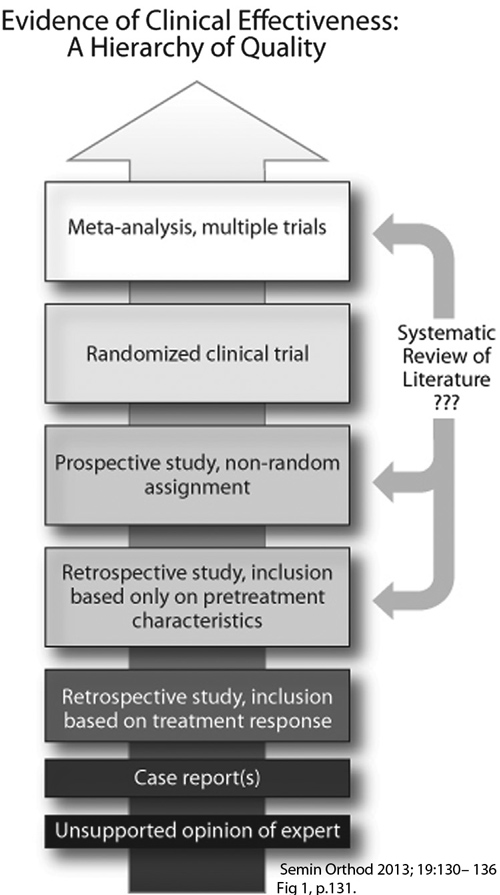 Drs Peter Dawson and Mark Piper's researches and work have to be placed, like it or not, in the "unsupported opinion of expert" category, at the bottom of the scale of scientific evidence. Holy Koh and Peter Robinson's article on occlusal adjustments from the Cochrane library is located at the top of the scale along with meta-analysis including multiple trials. I invite you to read the whole article: Occlusal adjustment for treating and preventing temporomandibular joint disorders (Review)
Drs Peter Dawson and Mark Piper's researches and work have to be placed, like it or not, in the "unsupported opinion of expert" category, at the bottom of the scale of scientific evidence. Holy Koh and Peter Robinson's article on occlusal adjustments from the Cochrane library is located at the top of the scale along with meta-analysis including multiple trials. I invite you to read the whole article: Occlusal adjustment for treating and preventing temporomandibular joint disorders (Review)
It is interesting to note that none of Drs Dawson and Piper's research work was selected in this meta-analysis. It is likely to believe that their work didn't meet the high selection criteria and absence of bias to be considered and included in the meta-analysis.
.
Mark Piper and "Piperism"
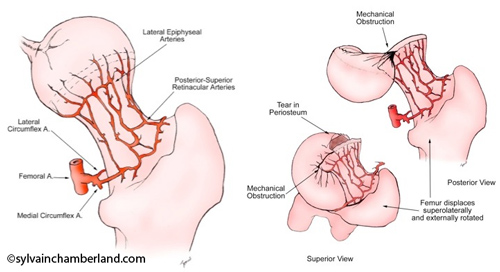
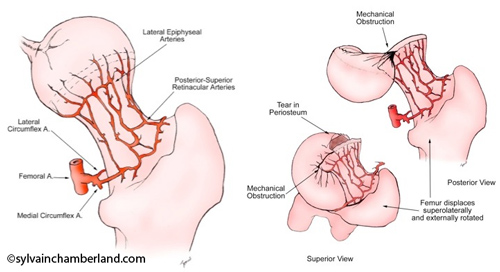
A very good example of preconceived idea is provided to us by Dr Mark Piper when he describes TMJ avascular necrosis by saying that compression of the TMJ perforating blood vessels occurred. He tries to link avascular necrosis caused by a fracture and collapse of the femoral head where a main artery and branches of lateral and medial circumflex femoral artery are located.

He pretends that anterior disc displacement compresses “so-called” TMJ perforating blood vessels and causes avascular necrosis of the condyle.
But this artery does not exist.
Piper uses avascular necrosis concept to promote his microsurgery technique where he perforates the head of the condyle to promote vascularization.
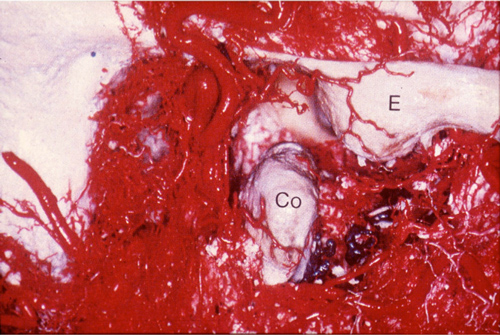
He showed histological bone cuts that he removed during these perforations while saying that "his pathologists" said that it was "dead" bone.
But when these samples were re-analyzed by
independent and renowned
pathologists, they all showed that the bone was alive and they refuted his whole avascular necrosis concept, which scientifically put an end to the discussion.
Piper's results concerning the use of adipose tissue grafts to treat TMJ internal derangements and condylar resorption
were never published in any renowned journal where articles are
revised by peers before publication (peer-review journal). To this day,
nobody has published an article showing that someone had been able to
reproduce Piper's results.
Definition of reproducibility in science
Reproducibility is the degree of similarity between measures or observations when reproducing a procedure, an experience, an analysis by different people in different places (hospitals, universities, countries). Reproducibility is part of the precision of the tested method.
Arterial blood supply of the TMJ
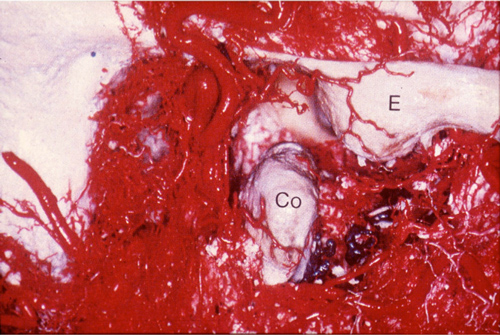
Arterial blood supply of the TMJ comes from multiple sources (external pterygoid muscle, cancellous bone, internal pterygoid muscle, posterior attachment vessels and transverse facial artery). Anybody having performed a surgery on a TMJ knows that blood supply comes from multiple sources. See the attached picture showing the arterial network and see Dr Carl Bouchard’s video clip while he performs a costochondral graft on one of my patients. Notice the hemorrhage when he unfortunately cuts a small artery when working on the left side (CCG link).
The Québec Association of Orthodontists recently invited Dr Alain Aubé to hear his point of view on TMJ. Let’s say that several colleagues from the Association expressed huge hesitations against the concepts conveyed by Dr Aubé. Numerous sophisms were noticed. We witnessed a display of preconceived ideas like we had rarely seen in a continuing education course.
We do not deny the use of magnetic resonance imaging in some TMJ pathologies, such as disc displacement, but diagnosis of TMD cannot be limited to magnetic resonance imaging.
Treatments of TMD have to rely on scientific basis.
Conclusion
The mistake to avoid is to put occlusion at the center of all TMJ problems and believe that the solution to TMJ problems is through only one functional occlusion model with canine guidance and bilateral contacts equally adjusted to 8-micron shimstocks.
Prevalence of Class I, Class II or Class III malocclusions is about equally distributed between men and women. Dismorphism is not based on gender.
Differences in types of malocclusions (Class I, Class II or Class III) exist depending on the population observed: white (Caucasian), Afro-American, Asian or Hispanic.
Incidence of TMD in the population in general is of 2 women for one man.
Incidence of patients suffering from TMD is of 10 women for one man.
Dr Larry Wolford (Atlas Oral Maxfacial Surgery Clin N Am 19 (2011) 243-270), in a research comprising 1369 consecutive patients from 8 to 76 years of age referred for TMD, observed a proportion of 78% of women and 22% of men. 69% of affected patients mention that their problem started in their teenage years. He concludes that TMD mainly develop in teenage girls.
We can think about the following:
If occlusion were the cause, it is likely to pretend that the M-F distribution would be more balanced.
In this context, isn't it unlikely to pretend that occlusal adjustment prevents TMD knowing that women are more affected by this kind of problem and that there are no differences between men and women in prevalence of malocclusions?
In conclusion, I will quote Dr Louis Mercuri:
"It is essential that TMJ osteoarthritis be presented as the pathologic entity it is in the same terms as our colleagues discuss osteoarthritis in orthopaedic circles.
To not do this only exacerbates the problem that everyone dealing with this entity patients, clinicians, insurance carriers, and so forth has with TMJ osteoarthritis, because they do not consider it as the orthopaedic (medical) pathology that it is, but rather a purely dental TMJ problem."
L.G. Mercuri Oral Max Surg Clin N Am 20 (2008) 169-183
Finally, I recommend to you the excellent book from Drs Charles Greene and Daniel Laskin which was just released to rectify a lot of your preconceived ideas that were transmitted to you by Drs Dawson and Piper.
Treatment of TMDs:
Bridging the gap between advances in research and clinical patient management, ©2013 Quintescence Publishing Co.